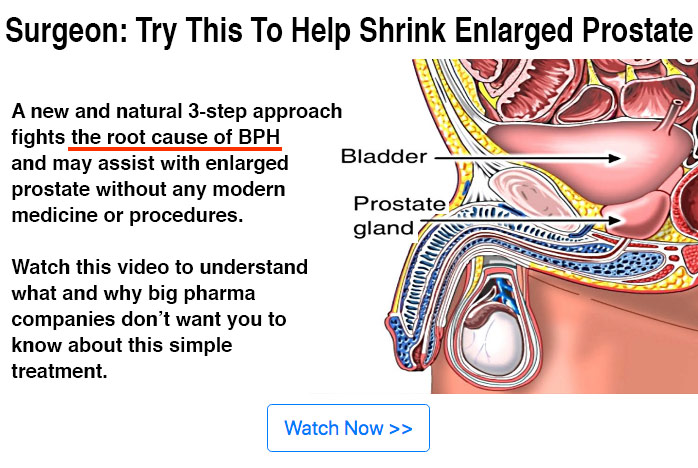
20 Lifestyle Choices Now Linked By Multiple Scientific Studies To INCREASED Cancer Risk Graphic © herbshealthhappiness.com
Background photo: Pixabay (PD)
Lifestyle Choices And Cancer Risk
Here’s my free report on 20 lifestyle choices linked to increased cancer risk! This is an in-depth, carefully researched, high quality report with over 75 scientific references. Please link to this page and hit the share button!
1 – Smoking
2 – Unsafe Sex
3 – Hormone Replacement Therapy
4 – Birth Control Pills
5 – Excessive Sun Exposure
6 – Not Maintaining Healthy Weight
7 – Prolonged Sitting
8 – Occupational Exposure
9 – Dry Cleaning Chemicals
10 – Night Shift Work
11 – Microwave Use
12 – CT scans
13 – Cellphone Use
14 – X-Rays
15 – Get Total Darkness While Sleeping
16 – Get Water Filtration
17 – Get Air Purification
18 – Take Regular Exercise
19 – Take A Daily Walk
20 – Get Early Screening
1 – Smoking
Smoking is a killer – and that’s a fact. The CDC declares the act of smoking as the number one risk factor for lung cancer, and hundreds of scientific studies have been published to back up this claim. Smoking cigarettes has been linked to as many as 90 percent of lung cancer cases in the United States, but other tobacco products have also contributed to lung cancer incidence – such as the use of cigars and pipes. Cigarette smokers are 30 times more likely to be diagnosed with lung cancer (or die from it!) compared to non-smokers. [1]
A recently published study by Underner, et. al. in 2015 further supported the claim of the dangers of smoking, finding that continued smoking has a continually negative impact on the progression and treatment of lung cancer. The researchers agree that smoking cessation is a vital part in the management of patients with lung cancer, in order to improve the quality of life. [2]
Smoking is not only linked to respiratory system cancers (the most obvious cancer to link it to) but other forms of cancer such as breast cancer. Boone, et. al. found that smoking was linked to increased incidences of breast cancer morbidity and mortality, regardless of other factors. Don’t forget secondhand smoke, which also increases the risk for certain types of lung cancer. In some ways, secondhand smoke is worse than smoking first hand because it includes unfiltered “sidestream” from the cigarette which exposes you to more toxic chemicals. [3][4]
Seeing as smoking is a modifiable risk factor with no actual health benefits, avoiding it completely is the best way to reduce your risk for cancer!
2 – Unsafe Sex
Safe sex is a must for sexually active people. In today’s day and age, the availability of items used in safe sex (e.g. condoms and diaphragms) has vastly improved. Despite that, the stigma placed on sexual activity has affected the choices young people make regarding their sexual health. Some STDs can lead to an increased cancer risk: The Human Papillomavirus or HPV is one of the biggest contributing factors to cancers that affect the cervix, vulva, vagina, penis, and anus (as well as oropharyngeal cancers) – and you can get it from unsafe sex. It is estimated that 14 million people in the US acquire an HPV-infection each year. [5] However note that very few people infected with HPV will develop cancer and in 90% of cases, the infection is cleared naturally by the body within 2 years. [6] HIV type 1, Hepatitis B and C are also listed by the IARC as group 1 “known carcinogens”. [7]
Getting HPV from unsafe sex is dangerous because viruses basically “hijack” cells, forcing them to create more viruses. This alone can cause cancer because the HPV virus changes the cells, and mutated cells are one of the many characteristics of cancer.
There are more than 100 types of HPV and around 15 are associated with cancer. HPV-types that classify as “high risk” because there is a higher risk for cancer when you are infected with them, include types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 66. [7] Women affected with cervical cancer can have multiple HPV-types in their cervical cells, according to Wang, et. al. [8]
Risk factors for HPV include: multiple sex partners, early age during first sexual intercourse, and practicing unsafe sex. A study has linked multiple sex partners with a higher-risk HPV, specifically unsafe oral sex. While abstaining may indeed be the best way to avoid cancers that affect the sexual organs of the body, safe sex should be practiced by people who are or are planning to be sexually active. You are not only protecting yourself, you are also protecting the health of your partner. It’s advisable to get tested for STDs regularly or whenever there was a potential exposure – in addition to actual safe sex practices.
You cannot get infected with HPV from toilet seats, skin contact, swimming, or sharing utensils. It isn’t hereditary either! [9]
3 – Hormone Replacement Therapy
Hormone replacement therapy (HRT) aka. menopausal hormone therapy (MHT) is a medical treatment that involves the introduction of hormones to the body in order to manage the signs and symptoms of menopause in women. Women who get HRT can do so via pill, skin patch, injections, cream, gel, or spray. The first three are the most popular ways this method is used and have proven effective. But this therapy comes with a price. While HRT is able to prevent the irregular periods, vaginal dryness and hot flashes that come with menopause – it can also increase your risk for cancer. [10][11]
There are conflicting results when it comes to studies about HRT and breast cancer risk. However, the fact that there are results of a significant associations between them means that we should be more cautious when choosing HRT to manage menopause. A study conducted in Norway from 2004 to 2009 (and published in 2015) concluded that HRT caused a majority of breast cancer cases in the population. Li, et. al. conducted a similar study in 2014 on different kinds of HRT, concluding that combined hormone therapy (CHT) increased breast cancer risk after three years of use. Estrogen hormone therapy (EHT) also caused an increased breast cancer risk, but after nine years of use. In fact, another study found that while exercise was able to reduce breast cancer risk, taking HRT cancelled out its protective effects. [12][13]
While hormone therapy can really help women suffering from menopause, it is also very risky. Like birth control pills, use of hormone therapy can cause rapid growth of breast tissue and formation of tumors – which increases the risk for various forms of breast cancer. [14]
There many alternative natural methods you can turn to in managing menopause (like green tea, ginseng, other herbs and soy) instead.
4 – Birth Control Pills
To many people, “the pill” has been a very effective family planning method – preventing unwanted pregnancies as well as regulating the body’s hormones. However, most people forget that these pills have both short-term and long-term side effects. BreastCancer.org has reported concerns that using hormonal contraceptive pills could also overstimulate the growth of breast cells, which could possibly contribute to an increased risk for breast cancer. While family history may also play a role in breast cancer, personal habits and medication use can also contribute to the cancer’s development. [15]
Recently, numerous studies have also had results that link birth control use with breast cancer. A significant study by Beaber, et. al. in 2014 concluded that use of oral contraceptives, both long-term and current use, was associated with an increased risk for breast cancer for women aged 20 to 44. Long-term use was described as 15 years or longer and current use was described as five years or longer. Lanfranchi’s 2014 study answered the Breast Cancer Organization’s concerns, wherein hormonal contraceptives increased breast cancer risk through its proliferative effect on breast tissue (which can cause tumor growth). There are many other studies that share the same results – this alone should cause anyone, male or female, to be concerned about breast cancer risk. [16][17]
To reduce your cancer risk, practice other methods of family planning instead of taking birth control pills.
5 – Excessive Sun Exposure
Getting a little sun is an important part of maintaining good health, but as beneficial as sunlight is, too much can also cause health problems. Sun exposure can cause skin cancer by damaging skin cells and causing mutation (and therefore cancer). The American Cancer Society cites skin cancer as the world’s most common cancer, with 5.4 million cases diagnosed every year, with UV exposure is one of the major risk factors in acquiring it. We need to protect ourselves by wearing or using appropriate gear. [18]
Nahar, et. al. published a study in 2015 concluding that low perceived risk and lack of knowledge regarding sun protection methods contributed greatly to non-melanoma skin cancer risk, especially among people who have been previously diagnosed with skin cancer. The fourth edition of the European Code published in 2015 advises against “too much sun, especially for children. Use sun protection. Do not use sunbeds” to reduce our exposure to harmful UV rays that contribute to skin cancer. [19][20]
Most people are unaware that sun exposure has also been linked to other cancers! Tyburczy, et. al. published a study in 2014 whose results showed that sun exposure caused second-wave cellular mutations in people affected by tuberous sclerosis complex (TSC), a condition where tumors form in different organ systems of the body. [21]
Because your skin can get damaged in as short as 15 minutes, the CDC advises everyone to practice adequate sun safety whether or not you live in a place that gets a lot of sun. There are five main tips to protect yourself from the sun: [22]
(1) Seek shade! Hide out under an umbrella, tree, or other shade cover to avoid that sun’s harmful rays.
(2) Pants and long-sleeved shirts are an excellent way to protect yourself, especially if they are made with tightly woven, dark colored fabric.
(3) Add a broad-brimmed hat or sun visor to your outfit. Your face is one of the most important areas of the body that needs protecting from the sun. The skin on the face is very sensitive and gets damaged very easily, additionally making you prone to wrinkles. Wide brimmed hats are the best kind of hats to wear for sun protection because they provide maximum shade for the face and back of the neck (one of the most common places to get sunburn).
(4) Don those sunglasses! Sunglasses protect your eyes from harmful UV rays and actually reduce the risk for cataracts. The bigger your sunglasses, the bigger the area of skin they cover. In fact, some sunglasses are coated to prevent UVA and UVB rays from reaching your eyes. According to Chorley, Evans, and Benwell in 2011, coated prescription glasses are effective in sun protection but sunglasses are still superior. [23]
(5) Be aware that reflected sunlight can also expose you to UV rays. Very fair skinned people may find that they can get sunburn even from reflected sunlight bouncing back from reflective surfaces such as concrete or white painted walls.
6 – Not Maintaining Healthy Weight
A healthy weight has always been linked with better health. Typically, people with normal body mass indices have a healthier diet and lifestyle compared to those who don’t.
Many studies have looked into causational relationships between weight gain and cancer, finding that the high body mass index was linked to a higher risk for several types of cancer:
– The results of Schlesinger, et. al.’s study in 2015 found that for every five kilogram increase in body weight, there was a four percent increase in colorectal cancer risk. This association was present no matter the age or sex of the person, although risk was higher for men. [24]
– According to Meyer, et. al. in 2015, weight alone did not contribute to an increase in cancer risk, but increased the risk significantly in people who smoked. [25]
– Stevens, et. al in 2014 focused on endometrial cancer risk and the age at which high body mass index contributed to it. The results revealed that high BMI at age 18 and subsequent gains in weight during adulthood were significantly associated with increase in endometrial cancer risk. [26]
– Suzuki and Saji’s study in 2015 showed that one of the reasons why menopause contributed to breast cancer risk is because of the weight gain that comes with fluctuating estrogen levels. An increase in body fat after menopause is linked to the formation of tumors in the breast, which can be malignant or cancerous. [27]
Keeping your BMI at normal levels (between 18 and 24) can greatly deter your risk for different cancers. Eat more vegetables, cut out sugar, avoid processed food, and exercise regularly!
7 – Prolonged Sitting
Having a sedentary lifestyle is one of the major risks factors that contribute to chronic cardiovascular and metabolic diseases like hypertension and diabetes, with recent studies showing how siting for long periods directly relates to cancer. Spending most of your time sitting down has actually been linked to an increased risk for cancer, according to research done by the American Cancer Society.
The American Cancer Society’s Cancer Prevention Study concluded that women who spent six or more hours sitting down had a 37 percent greater chance of mortality compared to women who sat down for three hours or less. The risk was lower for men (at 17 percent) but still present all the same. Exercise also factored in to the same study, wherein women who did not exercise and spent much of their time sitting down had an alarming 94 percent higher risk for death compared to men’s 48 percent. [28]
When it comes to site-specific cancers, Patel, et. al. in 2015 concluded that longer time spent sitting down was associated with higher total cancer risk in women for multiple myeloma, breast, and ovarian cancers. In men, Simons, et. al. in 2013 found that longer occupation sitting time increased the risk for colorectal cancer, and that increase in physical activity reduced this risk. [29][30]
If you have a job that entails hours on end doing desk work, maybe it’s time to find ways to be more active in the workplace. Take a ten to fifteen minute break every two hours or so to get your circulation moving and your muscles a short work out. This will also help prevent work burnout and reduce physical and mental stress associated with long work periods.
8 – Occupational Exposure
Occupational exposure is one of the most common risk factors in acquiring cancer. People who work with carcinogens that they would otherwise not be exposed to in their daily lives are at great risk for becoming diagnosed with a variety of cancers. Carcinogenic substances like coal tar pitch, creosote, arsenic, or radium are typically used in industrial processes where workers can become exposure to high quantities and raise their susceptibility to cancer.
Coal tar pitch is a by-product of industrial processes that use coal tar (such as aluminum production), and has been classified as a group one carcinogen by the IARC. The National Cancer Institute reports that occupational exposure to coal tar pitch has been linked to cancers of the skin, lung, bladder, kidney, and gastrointestinal tract. Another by-product of coal production is creosote, which is typically used in the wood industry. Spilled creosote can also become absorbed by groundwater and, eventually, plants. The IARC concludes that creosote is probably carcinogenic to humans because of reports linking it to skin and scrotal cancers. [31][32]
Other common substances that workers are exposed to include arsenic and radium. Arsenic exposure can come from places that manufacture pesticides and work with copper and in mining. The American Cancer Society reports that arsenic exposure causes increased risk and incidence in lung cancer, the longer a worker is exposed. Other cancers that can be linked to arsenic are bladder, kidney, lung, skin, colon, liver, and prostate cancers. Similarly, exposure to radium has, a radioactive chemical used in chemotherapy and is also a byproduct of coal and fuel production, has been linked to bone, liver, and breast cancer, according to the Agency for Toxic Substances and Disease Registry. [33][34]
These are just a few examples. Before choosing a career path, make sure to thoroughly check the health risks you may be exposed to!
9 – Dry Cleaning Chemicals
Dry cleaning is the preferred choice for many types of clothes that are too delicate to be washed in water. Instead of water, the dry cleaning process uses chemicals or solvents that do not harm fabric. However, while dry cleaning does make it easier to clean delicate clothes, the chemicals used can harm a person’s health. Recent studies have shown that a chemical involved in dry cleaning called “perc” or perchloroethylene is directly linked to several types of cancer. Either inhalation or direct contact with perchloroethylene (and variations of it) can cause an increase in cancer risk.
Vlaanderen, et. al. in 2014 found that tetrachloroethylene (TCE), another chemical used in dry cleaning, increased the risk for bladder cancer among dry cleaners. [35] The IARC has also classified this chemical as a probable carcinogen to humans. Perc, in particular, was also studied by Guyton in 2014. The results concluded that the chemical is likely to be carcinogenic, causing bladder cancer, non-Hodgkin’s lymphoma, and multiple myelomas. The same study also concluded that exposure to Perc caused neurotoxicity, or damage to the body’s nervous system. [36] Vlaanderen, et. al. also conducted an older study in 2013 on TCE and Perc, concluding that Perc exposure increased the risk for liver cancer and non-Hodgkin’s lymphoma. [37]
If you are having clothes dry cleaned, take care to avoid breathing any residual solvents and let the clothes air out completely before bringing them not your living space or wearing them.
10 – Night Shift Work
If you work in places such as medical institutions where business is ongoing 24/7, night shifts are unavoidable. Somebody has to work late hours and sometimes that person is you. However, disturbances in a person’s sleep pattern has been linked to different health problems – among them cancer! When a person loses sleep, it can affect their immune system and make them more susceptible to disease because sleep is when the body “recharges”. Lack of quality sleep causes problems in concentration, mood changes, and loss of energy – and apparently, cancer as well.
A 2015 study by Papantoniou, et. al. conducted a study on night shift work in Spain. The researchers concluded that overall risk for prostate cancer was higher for people who worked night shifts. And it doesn’t stop there! The risk for prostate cancer was high for people who worked mornings but used to work long-term night shifts beforehand, suggesting that exposure to night shift work at any point in time could increase your cancer risk and worsen your prognosis. [38]
For women, night shift work and poor quality sleep has been linked to increased breast cancer risk. In a study by Wang, et. al. in 2015, there were three sleep factors that interplay with each other to increase breast cancer risk significantly (compared to the factors independently): night shift work, long sleep durations, and lack of daytime napping. [39] A literature review was done previously in 2011 by Brudnowska and Pepłońska and focused on the effect of night shift work on risk for colorectal cancer, endometrial cancer, prostate cancer, and non-Hodgkin’s lymphoma. The association between breast cancer risk and night shift work was widely studied because of positive correlational results. [40]
If possible, try to avoid jobs that ask you to spend a lot of time in the night shift – especially if you still have to do work or run errands in the morning, leaving you no time for quality sleep. If you can’t 100 percent avoid working nights, try to get a full number of hours sleep later to give your body a chance to recover.
11 – Microwave Use
Frozen dinners and other microwave foods have become very popular to busy people or those who are willing to prioritize leisure time and sleep over slaving away in a hot kitchen to cook a meal. When it takes minutes to heat up leftovers or frozen pizza, using the microwave becomes more and more appealing.
While the “official” consensus is that microwaves to do not produce enough radiation to make food heated in them dangerous, there are several facts that warrant your attention. Microwave ovens produce radiation that allows water molecules in food to vibrate and create heat – which in turn heat food. Exposure to this type of radiation can cause mutations in cells and create cancer but in microwave ovens, this radiation is intended to be contained. However, microwaves are still electronic devices that wear and tear over time, and you cannot be 100 percent sure that it doesn’t leak radiation. [41]
It’s an ironic point that microwaves have been proven to be an effective cancer treatment – because they can cause cell-death! Different studies have shown how localized treatment with microwaves can kill cancer cells in breast and colorectal cancer. But remember, the possibility that your microwave is leaking radiation affects your healthy cells and can damage them. [42][43]
While you save time on cooking, you could be increasing your risk for cancer every time you choose the microwave instead of a stove. The radiation you expose yourself too can be minute, but would not be detectable until it’s too late.
12 – CT Scans
The advent of medical technology has brought about advancements that help with the diagnosis different medical conditions. However, there are many risks that come with using technology on our bodies – especially diagnostic examinations that use radiation. Exposure to radiation is a long-established risk factor for cancer, and studies have been done assessing the degree of risk associated with undergoing specific diagnostic procedures that involve the use of radiation. Radiation can cause mutations in healthy cells, which may lead to rapid growth and the development of cancerous tumors.
A French article published in 2016 delved into studies that focused on the effects of CT scan exposure in childhood on long-term cancer risk. The results found that there was an increase in cancer risk after several exposures to CT scans. Because children have weaker and immature immune systems, their healthy cells are more prone to mutation (when exposed to radiation) and therefore more prone to the development of cancer. Another study in 2016 by Berrington de Gonzales, et. al. also found a relationship between pediatric CT scans and risk for leukemia and brain tumors. Most of the studies you will find are for childhood exposure to radiation, but the risk for adults is still present. [44][45][46]
The National Cancer Institute states that the risk for cancer and exposure to CT scans is small and that the benefits usually outweigh the risks. However, the presence of the risk because of exposure to radiation should be understood. In fact, it is suggested that complete assessment of medical histories and examinations be done prior to a CT scan if reasonable to do so – as this may help reduce exposure to unwarranted procedures. It’s not the place of this guide to make a medical recommendation: Before agreeing to any medical procedure that involves radiation, discuss the risk with your physician first. [47][48]
13 – Cellphone Use
The use of mobile devices has increased exponentially in the last 20 years – and will likely continue to increase as affordable phones are marketed globally and network areas are expanded. With mobile phone subscriptions hitting close to an astonishing 7 billion globally, [49] our exposure to radio frequency electromagnetic fields (RF-EMF) is higher than ever. This has raised concerns regarding the effect of RF-EMF on humans, particularly their risk for cancer.
In 2011 the International Agency for Research on Cancer (IARC) classified RF-EMF as possibly carcinogenic, because of a higher risk for gliomas, a type of brain cancer. [50] Fully understanding how RF-EMF affects a person’s health needs further research and study in order to raise public awareness on the dangers of too much cell phone usage.
Radio frequency (RF) is emitted by all hand-held electronic devices, such as mobile phones, tablets, and laptops. Here is the bottom line: the IARC has published a statement that RF-EMF can cause cancer in humans, classifying it as “2B” which means several research publications have concluded that exposure to RF-EMF increases human risk for brain cancer, specifically gliomas. [50] This announcement was made only three years after the first iPhone was launched – from which the battle for the best smartphone begun, with companies like Samsung, Asus, and many others releasing smartphone after smartphone, typically six months to a year after their previous releases. Today, low-production costs in places like China have added more and more cellular phones to the market, drastically increasing human exposure to RF-EMF. [51]
According to Dindic, et. al’s review in 2013, cells that are exposed to RF-EMF experience high levels of oxidative stress. Because of this, free radicals become present in the blood, one of which is peroxynitrite, a very aggressive free radical that is able to break single-strand DNA – which can ultimately cause cancer. [52]
One of the most troubling recent studies explaining the risk of RF-EMF was published in the latter half of 2014 by Hardell and Carlberg. [53] Since the IARC study only covered a short latency period of 10 years, Hardell and Carlberg extended their study to include a 25-year period. Hardell and Carlberg’s results were conclusive – use of mobile and cordless phones were directly associated with increased risk for glioma, with the risk increasing the longer a person is exposed to RF-EMF. In fact, the group with greater than 25 years of mobile and cordless phone use had a three-fold increased risk compared to users with less than 12 months exposure to same devices. The researchers also published a further study in 2014 which revealed decreased survival rates with long-term mobile phone use among glioma patients. [54]
A study in 2004 revealed that mobile phone use of at least 10 years increased the risk of acquiring acoustic neuroma. [55] Another study in 2009 revealed a positive association between mobile phone us and the development of parotid gland tumors. [56] In 2013, Bhat, Kumar, and Gupta analyzed published studies on mobile phone use and cancer risk, concluding that long term, low intensity exposure to radiation from mobile devices could potentially lead to tumor formation. [57]
However, let’s be honest; we cannot easily just cut cell phone use out of our lives. But here are a few tips to help reduce your exposure and your cancer risk.
1) Limit the duration of cell phone use, especially long calls.
2) Keep a greater physical distance between the device and your head when on the phone. For example use speaker mode or a headset. Also it’s better if possible to have the phone turned up louder and held further away from your head during regular calling. Every inch further away may be helpful as the RF is strongest right next to the device.
3) Rather than keeping the phone in a pocket when not on a call, keep your phone in a bag or in another location not directly attached to your person. Smartphones are transmitting and receiving data even when you are not making a call.
4) Limit children’s access to mobile devices to scenarios where they would be valuable for increased safety.
14 – X-Rays
There is an important reason why pregnant women aren’t allowed to have their x-rays taken – because the radiation is powerful enough to harm an unborn fetus. The radiation from a simple x-ray is deemed safe for healthy adults and children. But take another read at that sentence – if x-rays are not safe enough to risk exposure to an unborn, how can they really be described as “safe” for adults? What about the medical technicians who operate the machine and may potentially be exposed to levels of radiation for long periods of time? Are they “safe” from the dangerous of radiation as well?
Various studies have focused on occupational radiation exposure, not just from medical devices but other scenarios that involve the use of radiation, and found that risk and x-ray exposure are correlated:
– A study conducted by Wang, t. al. in China on x-ray technicians revealed that increasing occupational exposure from x-rays caused increasing breast and esophagus cancer risk. They suggested prevention strategies were needed in order to bring down the levels of exposure these medical technicians face. [58]
– Similar results were found by Fournier, et. al.’s 2016 study: Where there is a decrease in cancer-related mortality as radiation exposure decreases. [59]
– According to Preston, D., et. al. there was a positive association between occupational radiation to the breast and breast cancer risk. [60]
Your job is one of the biggest factors that can affect your health, specifically the carcinogens that you are exposed to at work. Working directly with medical equipment that produces radiation exposes your cells to damage that can cause cancerous mutations. This is particularly dangerous for women, wherein different studies have linked occupational radiation to breast cancer. Before you decide on a career path, research and be aware of the occupational hazards involved. If you do choose to work with radiation, make sure you use the correct protective gear and carefully follow best practices for safety.
==============================
The first 14 of the list were things to avoid / do less of. The remaining 6 are things to do more of:
15 – Get Total Darkness While Sleeping
Now this might seem bizarre in a manual about cancer risks – but researchers have discovered that turning off the light when you sleep can actually help prevent cancer! Exposure to light directly affects the way the body produces melatonin, a hormone that helps regulate the body’s sleep cycle. When you sleep with the lights on, the body produces less melatonin – likewise, spending more time in the dark produces more of it. This can interfere with your sleep-wake cycle in a manner similar to the way travelers experience jet lag when moving across time zones. There have also been studies that link a decrease in melatonin production with breast cancer. [61]
According to Alonso-Gonzales, et. al. in 2016, an increase in melatonin production has a protective effect against breast cancer. When melatonin is produced by the body, it creates stability at the genetic level, helping prevent the occurrence of breast cancer cells. On the other hand, a decrease in melatonin production could increase a woman’s risk for breast cancer. A similar study was done previously in 2014 by Dumont and Paquet, concluding that the decrease in melatonin production due to working at night could probably contribute to an increase in cancer risk. In fact, Benabu, et. al. in 2015 concluded that there was a moderate increase in risk for breast cancer among women who worked nights (see our chapter on night shift work for more on this). [61][62][63]
This information puts a new view on bad sleeping habits and cancer risk. It turns out that leaving the light on while you sleep could potentially increase your risk for acquiring breast cancer, especially if you work night shifts often. In order to keep your breast cancer risk low (and to save energy), remember to turn off your light before going to bed, or use a smaller, dimmer night light instead. It is advised also to sleep regularly at the same time of night, during natural darkness hours as much as possible.
16 – Get Water Filtration
Public water supplies are typically treated with chemicals to get rid of microorganisms that make would otherwise make the water dangerous to drink. However, these chemicals have been associated with dangerous effects on health. Public water sources are usually treated with chlorine. However many people are completely unaware that this process can produce DBPs or disinfection byproducts. DBPs are toxic and considered carcinogens.
The most common DBPs formed after water treatment are trihalomethanes (THM) – generated as a byproduct when chlorine is added to water and decays the natural plant life, like algae, weeds, and leaves. The scariest part about THMs is that they are colorless, odorless, and tasteless – all the while being toxic. These characteristics mean that these dangerous chemicals are hard to detect – but can cause serious health issues when ingested. [64] Different studies have linked THMs with cancers of the bladder, colon, and rectum. Min and Min, et. al. in 2016 concluded that blood trihalomethane levels were significantly associated with total cancer mortality in adults. [65]
It’s bizarre to think that filtering your tap water can mean the difference between life and death! But scientific studies have supported this. It’s a reality.
Rahman, et. al. in 2014 found a positive association between THM exposure (specifically bromoform) and colorectal cancer in men (but not in women) after a five year period. Salas, et. al. published a study with similar results in the same year, but with bladder cancer risk. THM exposure had a strong positive association with urothelial bladder cancer risk. There are other studies that focus on how THM exposure causes an increase in general cancer risk. [66][67]
Whole House Water Filters:
The best way to protect yourself from the dangers of chlorinated water is by using a water filter in your home. Whole house water filters are placed at the point of entry where water enters your home’s pipes. That means you don’t need a filter for every faucet, you just need one! When installed, your entire home receives clean, filtered water.
Berkey Water Filters:
These are a more high-end product targeted towards the more health-conscious consumer who demands top quality results from filtering his or her drinking water.
The Berkey Filter utilizes a solid block of activated carbon, which has micropores that only permit very small molecules through. Nasty chemicals such as pesticides, heavy metals, solvents, chlorine and its byproducts and even viruses and bacteria are removed to over 99.99%.
I have been using one of these for several years. It’s fascinating to filter tap water which you thought was clear, through one of these systems and compare the color of the filtered water against the unfiltered – you will suddenly see the discoloration in your tap water that you did not even realize was there! I quickly noticed that all the chlorine smell and taste is gone too. This is a high quality filter that should be perfect for all your drinking and cooking water needs.
Berkey prides itself in a variety of filter systems – their most popular being the portable water systems. They have quite a few models that are “portable” – from the truly portable sports bottle (called “Sport Berkey”) to larger, stainless steel containers. These portable filter systems are great for hiking or camping outdoors where there are natural sources of water like rivers or streams to take water from. Another popular filter system is the Berkey Fluoride Water Filter, which filters out fluoride (which is a very common additive to public water sources) from your drinking water. Berkey even offers a shower filter, able to reduce chlorine, dirt, and and odor from shower water.
There are other water filtration systems you can choose from but Berkey is definitely among the best. While chlorinated water is able to reduce the number of dangerous microorganisms from public water sources, different studies (see previous chapter) have shown how DBPs or disinfection byproducts could potentially lead to a variety of cancers. You can see Berkey water filters on Amazon here.
17 – Get Air Purification
Volatile organic compounds or VOCs are “off-gassed” from innumerable industrially-created products. Paint, plywood, plastics, memory foam, photocopiers, resins and adhesives, pesticides, and so many other manufactured items exude small amounts of these chemicals – typically at the highest rate when the product is new and decreasing over time. We are also exposed to them through engine exhaust, tobacco smoke and more.
The risks associated with breathing these chemicals have been greatly increased by the modern lifestyle: Homes have been made very airtight in order to improve energy efficiency / temperature control, and of course the number of synthetic products in our immediate environment has increased massively in the last several decades. In short, modern indoor environments are VOC traps – and we spend much of our lives either in rooms or cars, breathing these toxins.
If it doesn’t seem that serious, consider that indoor air quality is now regarded as one of the top 5 risks to public health!
A wide range of VOCs are quite dangerous to health and are considered carcinogenic. The most risky examples of VOCs include formaldehyde, benzenes, chloroform, and acetaldehyde. Different scientific studies have concluded how these VOCs can contribute to increased cancer risk. [68]
– Formaldehyde exposure has been linked to DNA damage and the development of a blood cancer called leukemia. [69]
– Similarly, benzene exposure has also been associated with hematopoietic malignancies (blood cancers) like leukemia in both adults and children. In utero, early life, and work exposure to benzenes increased the risk for leukemia. [70][71]
– Research done by the CDC has found chloroform to be a potential carcinogen, causing liver and kidney cancer in animal test subjects. [72]
– Further research is still needed on the carcinogenic effects of acetaldehyde but studies have shown a possible link between the chemical and cancer risk. There was a reported increase in nasal and laryngeal tumor incidence in test subjects exposed to acetaldehyde, causing it to be classified as a probable human carcinogen. [73]
These VOCs may or may not give off a pungent odor but are typically colorless and hard to detect. This makes them even more dangerous because signs and symptoms of toxicity will only appear after a person has been exposed for a long period of time.
In order to protect yourself and your family, consider these two steps
1) get as much fresh air as possible. If you are in a natural environment this is simple – open windows and vents, and spend time outdoors.
2) Get a VOC (gas phase) air filter.
A huge number of people are in urban environments where opening windows is not necessarily going to help the problem! Consider using a VOC filter inside your home or workplace. There are different VOC filters available – either portable or HVAC. Note that gas phase air purification is different from HEPA. HEPA filters are particle filters – they remove dust, pollen, fiberglass, lint and so on. VOC filters typically use activated carbon, perhaps in conjunction with permanganate-impregnated alumina.
Another thing to note is that the amount of carbon used is going to affect the air scrubbing ability of the filter. So look for the volume / weight of activated carbon used in the filter as an indicator of quality. Some of the cheaper modern air purifiers use a very thin layer of carbon in association with the HEPA filter – well, they can now put “removes VOCs” on the promotional materials, but in reality it’s less effective than a 2″ thick layer of carbon.
One of the most reputable brands of VOC air purifier is IQAir – here’s a link to their products on Amazon.
If you have the construction skill and the kind of property that supports it, you can also consider HVAC-style air purification that utilizes heavy duty carbon filters such as these.
Note that these are typically utilized by horticultural systems (especially by weed growers!) because they have a very great ability to remove VOCs from air. This demonstrates their high effectiveness.
Use a carbon layer in conjunction with a HEPA filter – and be aware of the “sequence” of filtering:
Pre-filter ==> VOC filter ==> HEPA filter.
The HEPA filter is placed last in the chain because then it will catch any carbon dust that is released by the activated carbon. Note that I have not investigated building code requirements for HVAC systems so you would need to get consultation on this.
Final note – activated carbon has a lifespan when it comes to absorbing odors and VOCs. Once they are ‘full’ they will start to release the VOCs back into the air. In short, if the air purifier starts giving off a smell, then it is most likely time to replace the filter.
18 – Take Regular Exercise
Personal diet and physical activity, specifically regular exercise, are two lifestyle choices that play very big roles in how “healthy” a person is. While health organizations typically promote these healthy lifestyle choices in order to fight chronic diseases that affect the heart and the body’s metabolism, recent studies have also demonstrate mechanisms by which exercise helps prevent cancer.
The National Cancer Institute promotes regular exercise of at least 30 minutes each day for at least five days (or 150 minutes of moderate exercise in a week) to 20 minutes each day (for vigorous exercise) for at least three days. Based on information from different studies, the NCI concludes that regular physical activity can help reduce cancer risk by maintaining good energy balance, hormone levels, and normal body weight or body mass index. [74]
Recent studies also have similar conclusions, specifically in terms of breast, ovarian, and prostate cancer to name a few. In 2015, Schmitz, et. al. found that aerobic exercise helped reduce breast cancer risk in women because it reduced or blunted estrogen levels in the body. Similarly, Sturgeon, et. al in 2016 concluded that aerobic exercise in high-risk premenopausal women could decrease breast cancer risk by helping reduce body fat. Tai, et. al. in the same year concluded that regular exercise reduced the risk and mortality for prostate cancer. Nechuta, et. al. in 2015 conducted a study in 2015 whose findings show a reduction in total cancer risk among test subjects who performed regular exercise. [75][76][77][78]
If you have a few minutes to spare, spend at least half an hour each day exercising. You can directly head to the gym after work (or before work if you wake up early!) or exercise in the comforts of your own home. There are plenty of available exercise programs that can fit your lifestyle.
19 – Take A Daily Walk
Adequate exercise is an excellent way to keep off the extra pounds and maintain good cardiovascular health. It is able to improve the circulation of blood and lymph in the body, energy levels, wellbeing and overall mood – all factors that can contribute to better health and can significantly contribute to the body’s ability to fight out cancer or slow its progression. Different studies have also shown how exercise, specifically walking, is able to reduce cancer risk and mortality.
In 2014, Williams found that walking was able to reduce risk of brain cancer mortality among test subjects. In fact, brain cancer mortality was lower by a striking 42.5 percent for people who engaged in walking exercises compared to those who didn’t or scarcely exercised. The same researcher conducted a similar study in the same year and found that walking reduced kidney cancer risk, independent of other extraneous risk factors like smoking, body mass index, co-morbidities like hypertension and diabetes, and use of medication. In Japan, a study was conducted by Ukawa, et. al. and concluded that daily walking (and less time spent watching the television) could possibly reduce liver cancer risk. [79][80]
Walking, and other similar forms of exercise like running, cycling, and swimming, have all been proven to improve health, particularly in terms of cardiovascular and metabolic health, and more recently, how it can help fight serious chronic diseases like cancer. The American Heart Association recommends at least 150 minutes of moderate exercise (e.g. brisk walking or swimming) or 75 minutes of vigorous exercise (e.g. running, aerobics) each week. Whatever your lifestyle may be, always take a few minutes each day in order to help reduce your risk for cancer. The minimum of 150 minutes of walking can be divided into 30 minutes each day for five days – see it as an investment that will pay back in the long run. [81]
20 – Get Early Screening
According to the National Cancer Institute, the cancer burden has a very big impact on society. In 2016, an estimated 1.7 million new cases of cancer will be diagnosed in the USA alone, and with the mortality rate being roughly a third of this estimate – that’s close to 600,000 Americans dying each year after being diagnosed with cancer. The most common cancers to be diagnosed in 2016 are those that affect the breast, lung, bronchus, colon and rectum, bladder, skin, thyroid, kidney, renal pelvis, pancreas, endometrium, and blood (leukemia). [82]
Living a healthy lifestyle has always been the best piece of advice for any sort of disease, but we have to consider that genetics or heredity plays a significant role in a person’s risk for cancer and their diagnosis. Statements like “It runs in the family” can apply to cancer as well, especially for cases of breast and colorectal cancer. The American Cancer Society reports that the percentage of hereditary cancer cases is estimated to be around five to ten percent – so how do you fight your genes? [83]
The answer is simple – early screening. In families where several cases of cancer occur, early screening is of paramount importance. A very important diagnostic characteristic for hereditary cancer is that the onset is early – with symptoms possibly showing up in a person’s early twenties. There are different types of screening tests available today, each one recommended by different health organizations to reduce mortality rates due to cancer: [84]
– Colonoscopy, sigmoidoscopy, and high-sensitivity fecal occult blood tests for colorectal cancer
– Low-dose helical computed tomography for lung cancer
– Mammography for breast cancer
– Pap smear and Human papillomavirus (HPV) testing for cervical cancer
The best way to fight cancer is to be prepared – and that involves spending more time on and giving more attention to your health. While you may find yearly check-ups and periodical examinations too bothersome, especially if you receive a negative result, remember that it is better to know for sure that you don’t have cancer than to receive a diagnosis late in your life when the disease was progressed too far to treat. Better to be safe than sorry! Visit your doctor to get an idea of which early screening tests best apply to you.
A study was conducted by RAND Corporation and found that doctors with less experience had higher cost profiles than doctors with more experience. This suggests that less-experienced physicians order more tests and procedures in order to reach a diagnosis – which is taxing on both the patient and the health care system. [85]
Of course, there are also studies that have concluded that experience or length in service is not the only factor to consider in labeling someone a “good doctor”. As with any profession, there will always be some who excel.
=====================================================
References:
[1] Centers for Disease Control and Prevention. What Are the Risk Factors for Lung Cancer? https://www.cdc.gov/cancer/lung/basic_info/risk_factors.htm
[2] Underner M, Perriot J, et al. (2015). Influence of tobacco smoking on quality of life in patients with lung cancer. Influence of tobacco smoking on quality of life in patients with lung cancer. https://pubmed.ncbi.nlm.nih.gov/26231411/
[3] Boone SD, Baumgartner KB, et al. (2015). Active and passive cigarette smoking and mortality among Hispanic and non-Hispanic white women diagnosed with invasive breast cancer. https://pubmed.ncbi.nlm.nih.gov/26387598/
[4] Kim CH, Lee YC, et al. (2014). Exposure to secondhand tobacco smoke and lung cancer by histological type: a pooled analysis of the International Lung Cancer Consortium (ILCCO). https://pubmed.ncbi.nlm.nih.gov/24615328/
[5] American Cancer Society. HPV and HPV Testing. https://www.cancer.org/healthy/cancer-causes/infectious-agents/hpv.html
[6] NHS “Can Oral Sex Give You Cancer” https://web.archive.org/web/20190414202309/https://www.nhs.uk/live-well/sexual-health/can-oral-sex-give-you-cancer/
[7] IARC Group 1 Carcinogens – via Wikipedia https://en.wikipedia.org/wiki/IARC_group_1
[8] Wang L, Wang P, et al. (2016). Prevalence of High-Risk Human Papillomavirus (HR-HPV) Genotypes and Multiple Infections in Cervical Abnormalities from Northern Xinjiang, China. https://pubmed.ncbi.nlm.nih.gov/27494179/
[9] Orosco RK, Kedarisetty S, et al. (2016). Predictors of high-risk and low-risk oral HPV infection in the United States. https://pubmed.ncbi.nlm.nih.gov/26707355/
[10] National Cancer Institute. Menopausal Hormone Therapy and Cancer. https://www.cancer.gov/about-cancer/causes-prevention/risk/hormones/mht-fact-sheet
[11] Mayo Clinic. Hormone therapy: Is it right for you? mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372
[12] Suhrke P & Zahl PH. (2015). Breast cancer incidence and menopausal hormone therapy in Norway from 2004 to 2009: a register-based cohort study. https://pubmed.ncbi.nlm.nih.gov/25991514/
[13] Li CI, Daling JR, et al. (2014). Use of menopausal hormone therapy and risk of ductal and lobular breast cancer among women 55-74 years of age. https://pubmed.ncbi.nlm.nih.gov/24748570/
[14] Pizot C, Boniol M, et al. (2016). Physical activity, hormone replacement therapy and breast cancer risk: A meta-analysis of prospective studies. https://pubmed.ncbi.nlm.nih.gov/26687833/
[15] Breastcancer.org. Is There a Link Between Birth Control Pills and Higher Breast Cancer Risk? https://www.breastcancer.org/research-news/study-questions-birth-control-and-risk
[16] Beaber EF, Malone KE, et al. (2014). Oral contraceptives and breast cancer risk overall and by molecular subtype among young women. https://pubmed.ncbi.nlm.nih.gov/24633144/
[17] Lanfranchi A. (2014). Normal breast physiology: the reasons hormonal contraceptives and induced abortion increase breast-cancer risk. https://pubmed.ncbi.nlm.nih.gov/25189013/
[18] American Cancer Society. Skin Cancer. https://www.cancer.org/cancer/skin-cancer.html
[19] Nahar VK, Ford MA, et al. (2015). Sun-related behaviors among individuals previously diagnosed with non-melanoma skin cancer. https://pubmed.ncbi.nlm.nih.gov/26515833/
[20] Greinert R, de Vries E, et al. (2015). European Code against Cancer 4th Edition: Ultraviolet radiation and cancer. https://pubmed.ncbi.nlm.nih.gov/26096748/
[21] Tyburczy ME, Wang JA, et al. (2014). Sun exposure causes somatic second-hit mutations and angiofibroma development in tuberous sclerosis complex. https://pubmed.ncbi.nlm.nih.gov/24271014/
[22] Centers for Disease Control and Prevention. Skin Cancer. https://www.cdc.gov/cancer/skin/basic_info/sun-safety.htm
[23] Chorley AC, Evans BJ, & Benwell MJ. (2011). Civilian pilot exposure to ultraviolet and blue light and pilot use of sunglasses. https://pubmed.ncbi.nlm.nih.gov/21888274/
[24] Schlesinger S, Lieb W et al. (2015). Body weight gain and risk of colorectal cancer: a systematic review and meta-analysis of observational studies. https://pubmed.ncbi.nlm.nih.gov/25925734/
[25] Meyer J, Rohrmann S, et al. (2015). Impact of Smoking and Excess Body Weight on Overall and Site-Specific Cancer Mortality Risk. https://pubmed.ncbi.nlm.nih.gov/26215293/
[26] Suzuki R & Saji S. (2015). Leanness, obesity, and breast cancer risk-different impact of body weight on breast cancer risk according to women’s life stages. https://pubmed.ncbi.nlm.nih.gov/25981644/
[27] Stevens VL, Jacobs EJ, et al. (2014). Body weight in early adulthood, adult weight gain, and risk of endometrial cancer in women not using postmenopausal hormones. https://pubmed.ncbi.nlm.nih.gov/24381074/
[28] American Cancer Society. Don’t Just Sit There. https://web.archive.org/web/20200329091130/https://www.cancer.org/latest-news/dont-just-sit-there.html
[29] Patel AV, Hildebrand JS, et al. (2015). Leisure-Time Spent Sitting and Site-Specific Cancer Incidence in a Large U.S. Cohort. https://pubmed.ncbi.nlm.nih.gov/26126627/
[30] Simons CC, Hughes LA, et al. (2013). Physical activity, occupational sitting time, and colorectal cancer risk in the Netherlands cohort study. https://pubmed.ncbi.nlm.nih.gov/23420352/
[31] National Cancer Institute. Coal Tar and Coal-Tar Pitch. https://www.cancer.gov/about-cancer/causes-prevention/risk/substances/coal-tar
[32] Agency for Toxic Substances and Disease Registry. ToxFAQsTM for Creosote. https://wwwn.cdc.gov/TSP/ToxFAQs/ToxFAQsDetails.aspx?faqid=65&toxid=18
[33] American Cancer Society. ToxFAQsTM for Arsenic. https://wwwn.cdc.gov/TSP/ToxFAQs/ToxFAQsDetails.aspx?faqid=19&toxid=3
[34] Agency for Toxic Substances and Disease Registry. ToxFAQsTM for Radium. https://wwwn.cdc.gov/TSP/ToxFAQs/ToxFAQsDetails.aspx?faqid=790&toxid=154
[35] Vlaanderen J, Straif K, et al. (2014). Tetrachloroethylene exposure and bladder cancer risk: a meta-analysis of dry-cleaning-worker studies. https://pubmed.ncbi.nlm.nih.gov/24659585/
[36] Guyton KZ, Hogan KA, et al. (2014). Human health effects of tetrachloroethylene: key findings and scientific issues. https://pubmed.ncbi.nlm.nih.gov/24531164/
[37] Vlaanderen J, Straif K, et al. (2013). Occupational exposure to trichloroethylene and perchloroethylene and the risk of lymphoma, liver, and kidney cancer in four Nordic countries. https://pubmed.ncbi.nlm.nih.gov/23447073/
[38] Papantoniou K, Castaño-Vinyals G, et al. (2015). Night shift work, chronotype and prostate cancer risk in the MCC-Spain case-control study. https://pubmed.ncbi.nlm.nih.gov/25530021/
[39] Wang P, Ren FM, et al. (2015). Night-shift work, sleep duration, daytime napping, and breast cancer risk. https://pubmed.ncbi.nlm.nih.gov/25794454/
[40] Brudnowska J & Pepłońska B. (2011). Night shift work and cancer risk: a literature review. https://pubmed.ncbi.nlm.nih.gov/21870422/
[41] American Cancer Society. Microwaves, Radio Waves, and Other Types of Radiofrequency Radiation. https://www.cancer.org/healthy/cancer-causes/radiation-exposure/radiofrequency-radiation.html
[42] Basile A, Failla G, et al. (2014). The use of microwaves ablation in the treatment of epiphyseal osteoid osteomas. https://pubmed.ncbi.nlm.nih.gov/23989501/
[43] Eng OS, Tsang AT, et al. (2015). Outcomes of microwave ablation for colorectal cancer liver metastases: a single center experience. https://pubmed.ncbi.nlm.nih.gov/25557924/
[44] Baysson H, Journy N, et al. (2016). Exposure to CT scans in childhood and long-term cancer risk: A review of epidemiological studies. https://pubmed.ncbi.nlm.nih.gov/26782078/
[45] American Cancer Society. Medical radiation. https://www.cancer.org/healthy/cancer-causes/radiation-exposure/x-rays-gamma-rays/how-are-people-exposed.html
[46] Berrington de Gonzalez A, Salotti JA, et al. (2016). Relationship between paediatric CT scans and subsequent risk of leukaemia and brain tumours: assessment of the impact of underlying conditions. https://pubmed.ncbi.nlm.nih.gov/26882064/
[47] National Cancer Institute. Computed Tomography (CT) Scans and Cancer. https://www.cancer.gov/about-cancer/diagnosis-staging/ct-scans-fact-sheet
[48] Schwartz D. (2008). Counter-Point: Are We Really Ordering Too Many CT Scans? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2672242/
[49] World Health Organization. Electromagnetic fields and public health: mobile phones. (2014).
[50] International Agency for Research on Cancer. IARC Classifies Radiofrequency Electromagnetic Fields As Possibly Carcinogenic To Humans. (2011). https://www.iarc.who.int/wp-content/uploads/2018/07/pr208_E.pdf
[51] Baan R, Grosse Y, et al. (2011). Carcinogenicity of radiofrequency of electromagnetic fields. https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(11)70147-4/fulltext
[52] Đinđić B, Radovanović Z, et al. (2013). Cytogenetic Damages Induced by Chronic Exposure to Microwave Non-ionizing Radiofrequency Fields. https://doaj.org/article/8b61d8fbb36a410ba84d0a4cea6759b9
[53] Hardell L & Carlberg M. (2015). Mobile phone and cordless phone use and the risk for glioma – Analysis of pooled case-control studies in Sweden, 1997-2003 and 2007-2009. https://www.sciencedirect.com/science/article/abs/pii/S0928468014000649
[54] Hardell L & Carlberg M. (2014). Decreased survival of glioma patients with Astrocytoma Grave IV Associated with Long-Term Use of Mobile and Cordless Phones. https://www.mdpi.com/1660-4601/11/10/10790
[55] Lönn S, Ahlbom A, et al. (2004). Mobile Phone Use and the Risk of Acoustic Neuroma. https://journals.lww.com/epidem/Fulltext/2004/11000/Mobile_Phone_Use_and_the_Risk_of_Acoustic_Neuroma.3.aspx
[56] Sadetzki S, Chetrit A, et al. (2007). Cellular Phone Use and Risk of Benign and Malignant Parotid Gland Tumors – A Nationwide Case-Control Study. https://academic.oup.com/aje/article/167/4/457/233171
[57] Bhat MA, Dr. Kumar V & Dr. Gupta GK. (2013). Exposure of Electromagnetic Radiation from Mobile Phone Communication Systems for Long Time Provokes Cancer Growth. https://www.journalijar.com/uploads/2013-09-03_142833_123.pdf
[58] Wang FR, Fang QQ, et al. (2015). Nested Case-control Study of Occupational Radiation Exposure and Breast and Esophagus Cancer Risk among Medical Diagnostic X Ray Workers in Jiangsu of China. https://pubmed.ncbi.nlm.nih.gov/26107226/
[59] Fournier L, Laurent O, et al. (2016). External radiation dose and cancer mortality among French nuclear workers: considering potential confounding by internal radiation exposure. https://pubmed.ncbi.nlm.nih.gov/27383840/
[60] Preston DL, Kitahara CM, et al. (2016). Breast cancer risk and protracted low-to-moderate dose occupational radiation exposure in the US Radiologic Technologists Cohort, 1983-2008. https://pubmed.ncbi.nlm.nih.gov/27623235/
[61] Hill SM, Belancio VP, et al. (2015). Melatonin: an inhibitor of breast cancer. https://pubmed.ncbi.nlm.nih.gov/25876649/
[62] Dumont M & Paquet J. (2014). Progressive decrease of melatonin production over consecutive days of simulated night work. https://pubmed.ncbi.nlm.nih.gov/25222345/
[63] Benabu JC, Stoll F, et al. (2015). Night work, shift work: Breast cancer risk factor? https://pubmed.ncbi.nlm.nih.gov/26597486/
[64] National Environmental Services Center. What are trihalomethanes? https://web.archive.org/web/20180328200102/http://www.nesc.wvu.edu/ndwc/articles/qanda/otsp99_q_a.pdf
[65] Min JY & Min KB. (2016). Blood trihalomethane levels and the risk of total cancer mortality in US adults. https://pubmed.ncbi.nlm.nih.gov/26840521/
[66] Rahman MB, Cowie C, et al. (2014). Colon and rectal cancer incidence and water trihalomethane concentrations in New South Wales, Australia. https://pubmed.ncbi.nlm.nih.gov/24938491/
[67] Salas LA, Villanueva CM, et al. (2014). LINE-1 methylation in granulocyte DNA and trihalomethane exposure is associated with bladder cancer risk. https://pubmed.ncbi.nlm.nih.gov/25482586/
[68] Indoor Air Quality (IAQ) Scientific Findings Resource Bank. VOCs and Cancer. https://iaqscience.lbl.gov/vocs-and-cancer
[69] Yu R, Lai Y, et al. (2015). Formation, Accumulation, and Hydrolysis of Endogenous and Exogenous Formaldehyde-Induced DNA Damage. https://pubmed.ncbi.nlm.nih.gov/25904104/
[70] Linet MS, Yin SN, et al. (2015). A retrospective cohort study of cause-specific mortality and incidence of hematopoietic malignancies in Chinese benzene-exposed workers. https://pubmed.ncbi.nlm.nih.gov/25944549/
[71] Carlos-Wallace FM, Zhang L, et al. (2016). Parental, In Utero, and Early-Life Exposure to Benzene and the Risk of Childhood Leukemia: A Meta-Analysis. https://pubmed.ncbi.nlm.nih.gov/26589707/
[72] Agency for Toxic Substances and Disease Registry. ToxFAQsTM for Chloroform. https://wwwn.cdc.gov/TSP/ToxFAQs/ToxFAQsDetails.aspx?faqid=52&toxid=16
[73] United States Environmental Protection Agency. Acetaldehyde. https://www.epa.gov/sites/default/files/2016-09/documents/acetaldehyde.pdf
[74] National Cancer Institute. Physical Activity and Cancer. https://www.cancer.gov/about-cancer/causes-prevention/risk/obesity/physical-activity-fact-sheet
[75] Schmitz KH, Williams NI, et al. (2015). Dose-response effects of aerobic exercise on estrogen among women at high risk for breast cancer: a randomized controlled trial. https://pubmed.ncbi.nlm.nih.gov/26510851/
[76] Sturgeon K, Digiovanni L, et al. (2016). Exercise-Induced Dose-Response Alterations in Adiponectin and Leptin Levels Are Dependent on Body Fat Changes in Women at Risk for Breast Cancer. https://pubmed.ncbi.nlm.nih.gov/27197293/
[77] Tai SY, Hsieh HM, et al. (2016). Hair dye use, regular exercise, and the risk and prognosis of prostate cancer: multicenter case-control and case-only studies. https://pubmed.ncbi.nlm.nih.gov/26996776/
[78] Nechuta SJ, Shu XO, et al. (2015). Adolescent exercise in association with mortality from all causes, cardiovascular disease, and cancer among middle-aged and older Chinese women. https://pubmed.ncbi.nlm.nih.gov/26231350/
[79] Williams PT. (2014). Reduced risk of brain cancer mortality from walking and running. https://pubmed.ncbi.nlm.nih.gov/24091993/
[80] Ukawa S, Tamakoshi A, et al. (2014). Associations of daily walking and television viewing time with liver cancer mortality: findings from the Japan Collaborative Cohort Study. https://pubmed.ncbi.nlm.nih.gov/24728669/
[81] American Heart Association. American Heart Association Recommendations for Physical Activity in Adults. https://www.heart.org/en/healthy-living/fitness/fitness-basics/aha-recs-for-physical-activity-in-adults
[82] National Cancer Institute. Cancer Statistics. https://www.cancer.gov/about-cancer/understanding/statistics
[83] American Cancer Society. Family Cancer Syndromes. https://www.cancer.org/healthy/cancer-causes/genetics/family-cancer-syndromes.html
[84] National Cancer Institute. Screening tests. https://www.cancer.gov/about-cancer/screening/screening-tests
[85] Mehrotra A, Reid R, et al. (2012). Physicians with the Least Experience Have Higher Cost Profiles Than Do Physicians with the Most Experience. https://www.rand.org/pubs/external_publications/EP51161.html
★ Get My Books - 100% FREE:
😳 Tinnitus And Brain Health?
After 47 years of studies and countless brain scans done on more than 2,400 tinnitus patients, scientists at the MIT Institute found that in a shocking 96% of cases, tinnitus was actually shrinking their brain cells.
As it turns out, tinnitus and brain health are strongly linked.
Even more interesting: The reason why top army officials are not deaf after decades of hearing machine guns, bombs going off and helicopter noises…
Is because they are using something called "the wire method", a simple protocol inspired by a classified surgery on deaf people from the 1950s...
★ How To Get Rid Of Nail Fungus:
★ Does Your Salad Contain This Vegetable?
★ 20 Natural Painkillers In Your Kitchen (Video):
★ Men's Prostate Health:
2. Famous Chef Sheds 60lbs Researching New Paleo Recipes: Get The Cookbook FREE Here
3. #1 muscle that eliminates joint and back pain, anxiety and looking fat
4. 7 odd foods that KILL your abdominal fat (surprising fat-fighters)
5. The TRUTH about bread (Will surprise you!)
6. [PROOF] Reverse Diabetes with a "Pancreas Jumpstart"
7. Here's What Happens When You "Unlock Your Hip Flexors"
8. The #1 WORST food that CAUSES Faster Aging (beware -- Are you eating this?)
The #1 Muscle That Eliminates Joint And Back Pain, Anxiety And Looking Fat
By Mike Westerdal CPT
Can you guess which muscle in your body is the #1 muscle that eliminates joint and back pain, anxiety and looking fat?
This is especially important if you spend a significant amount of time sitting every day (I do, and this really affects me in a big way!)
Working this "hidden survival muscle" that most people are simply not training because no-one ever taught them how will boost your body shape, energy levels, immune system, sexual function, strength and athletic performance when unlocked.
If this "hidden" most powerful primal muscle is healthy, we are healthy.
Is it...
a) Abs
b) Chest
c) Glutes
d) Hip Flexors
Take the quiz above and see if you got the correct answer!
P.S. Make sure you check out this page to get to know the 10 simple moves that will bring vitality back into your life:
If you enjoyed this page: