How To Shrink ENLARGED PROSTATE in 7 Easy Steps Graphic © herbshealthhappiness.com Background image: Shutterstock #1310215855 (under license)
According to the National Institute of Diabetes and Digestive Kidney Disease (NIDDK), more than 14 million men in the U.S. have an enlarged prostate. The risk appears to increase as we age—with the prevalence estimated at 50% among men older than 50 and 90% in 80-year-olds. [1]
A healthy prostate is important for all men! But as we age—and due to several risk factors we will discuss in this article—you may experience issues such as benign prostatic hyperplasia (BPH), which is basically an enlarged prostate.
BPH may lead to unpleasant symptoms that adversely affect a man’s quality of life. And due to the condition’s prevalence, it helps to know the warning signs, the causes, and how to solve the issue. Family physician Ken D. Berry, MD, covers this topic and recommends 7 easy strategies to shrink an enlarged prostate.
Signs Of An Enlarged Prostate
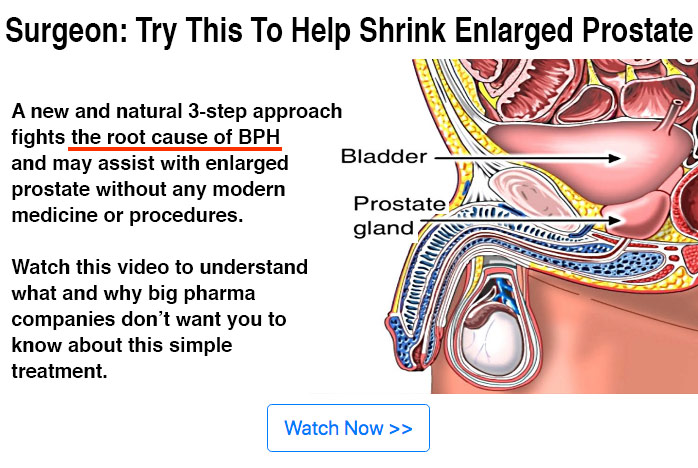
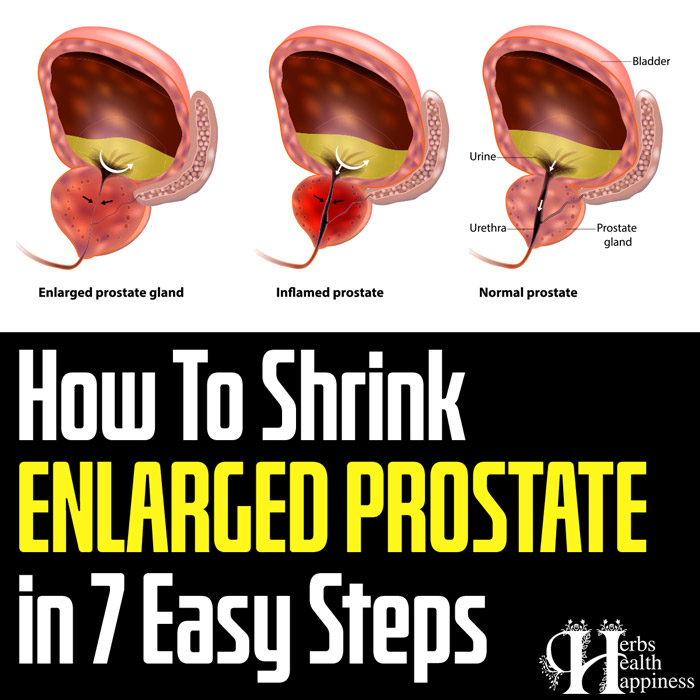
The prostate is a gland in the male reproductive system positioned just below the bladder. It’s responsible for a number of functions, including the production of seminal fluid and hormone metabolism. [2][3]
Due to its positioning in the pelvis, an enlarged prostate may squeeze and clamp down on the urethra. This is a tube that empties the bladder during urination. Due to the blockage, it becomes harder to pass urine, and the bladder may be overworked.
Some symptoms of an enlarged or benign prostatic hyperplasia include:
• Urinating frequently, during the day and at night (nocturia)
• Trouble delaying urination
• An interrupted or weak urine stream
• Incontinence (leakage or accidental urination)
• Urinary retention and difficulty starting a urine stream
• Incomplete emptying of the bladder and dribbling at the end of a stream
• Pain during urination or after ejaculation
• Urine with an odd smell or color
• Urinary tract infections
People with an enlarged prostate may not always experience these symptoms. But if you do, it’s advisable to talk to your doctor for a proper diagnosis.
Causes Of An Enlarged Prostate
Most men will develop an enlarged prostate in their lifetime. Aside from age, other risk factors for BPH include family history, inactivity, and obesity. [4][5][6]
And according to Dr. Berry, hyperinsulinemia (high insulin) may be a significant risk factor for BPH that doesn’t get enough attention. He references several studies that show a link between hyperinsulinemia and an increased risk of an enlarged prostate. [7][8][9][10][11]
But how does insulin affect the prostate gland? One mechanism may be through the stimulation of insulin-like growth factor 1 (IGF-1).
High insulin levels may stimulate the increased production of insulin-like growth factor 1 (IGF-1) in the liver. IGF-1, in turn, promotes the enlargement of the prostate. Elevated insulin may also reduce the synthesis of insulin-like growth factor binding protein-3 (IGFBP-3), which has inhibitory effects on growth. [12]
7 Steps To Shrink An Enlarged Prostate
Making healthy diet choices can help improve the health of your prostate. Dr. Berry argues that eating right is a simple and effective way to shrink an enlarged prostate. Some strategies to manage symptoms and the progression of BPH include.
1. Avoiding Sugar
We’ve seen that hyperinsulinemia may trigger enlargement of the prostate. So it only makes sense to lower your insulin level to reduce the risk of this happening. And in that case, cutting sugar from your diet should be the first thing on your agenda.
Whether it’s added sugars or fructose (natural sugar in honey and fruits)—Dr. Berry recommends avoiding all types of sugar. Research shows that a diet high in sugars may lead to a spike in insulin levels. [13][14][15][16]
2. Avoiding Grains
Still on the idea of reducing insulin levels to manage an enlarged prostate, it might be important to watch your intake of grains. Most studies point to refined or processed grain products such as pasta, rice, and white bread as significant risk factors for increased insulin levels. [17][18][19][20] But Dr. Berry adds whole grain foods such as wheat and oats to this list since they’re also converted into sugar.
3. Avoiding Soy
Soy contains phytonutrients known as isoflavones. They resemble estrogen, the female sex hormone— and are thought to mimic the effects of human estrogen to some degree. And by potentially increasing the level of estrogen in the male body, the compounds may inhibit testosterone production. [21]
According to some studies, the increase in estrogen and decrease in testosterone from soy consumption may play a role in promoting the enlargement of the prostate. [22][23][24][25]
4. Avoiding Low-Fat Dairy
An intake of full-fat dairy—and not low-fat—may reduce your risk of high insulin levels and help manage your enlarged prostate symptoms. And while research is conflicting on the effects of dairy on insulin levels, several studies show a connection. [26][27][28]
5. Avoiding Vegetable Seed Oil
The issue with vegetable seed oils is that most of them appear to have high omega-6 content. This includes sunflower oil, corn oil, soybean oil, rice bran oil, and cottonseed oil. A high intake of omega-6 may contribute to an increased risk of chronic inflammation—and potentially prostate enlargement. [29]
It’s worth noting that omega-3s found in fatty fish may positively affect hyperinsulinemia and BPH by reducing insulin levels. [30][31][32]
6. Eating a Low Carb Diet Such as Keto
Again, your eating habits play a key role in managing an enlarged prostate. In this case, it’s the diet plan you follow. Several studies suggest that lower-carb diet plans such as keto, Atkins, and the Mediterranean diet effectively increase insulin sensitivity and lower insulin levels. [33][34][35]
7. Intermittent Fasting
In a nutshell, intermittent fasting involves allocating specific hours for fasting and eating within the day. It’s mostly pushed for its potential weight loss benefits—but some studies indicate that intermittent fasting may also be effective at reducing your insulin levels. [36][37]
Other Ways To Shrink An Enlarged Prostate
In addition to the 7-step dietary strategy by Dr. Berry, several supplemention solutions may offer relief for an enlarged prostate. Some common options include saw palmetto, beta-sitosterol, pygeum, stinging nettle, and rye grass pollen extract. [38][39][40][41][42]
Dr. Berry concludes by insisting that BPH is a gradual process that takes years to develop. As such, don’t expect instant results from implementing his 7-step remedy or supplementation; this too will be a gradual process.
=====================================================
References:
[1] National Institute of Diabetes and Digestive Kidney Disease (NIDDK): https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia
[2] Lawrentschuk, N., Ptasznik, G., & Ong, S. (2021). Benign prostate disorders. Endotext [Internet]: https://www.ncbi.nlm.nih.gov/books/NBK279008/
[3] Swerdloff, R. S., Dudley, R. E., Page, S. T., Wang, C., & Salameh, W. A. (2017). Dihydrotestosterone: biochemistry, physiology, and clinical implications of elevated blood levels. Endocrine reviews, 38(3), 220-254: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6459338/
[4] Giri, A., Edwards, T. L., Motley, S. S., Byerly, S. H., & Fowke, J. H. (2015). Genetic determinants of metabolism and benign prostate enlargement: associations with prostate volume. PloS one, 10(7), e0132028: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4497718/
[5] Ngai, H. Y., Yuen, K. K. S., Ng, C. M., Cheng, C. H., & Chu, S. K. P. (2017). Metabolic syndrome and benign prostatic hyperplasia: an update. Asian journal of urology, 4(3), 164-173: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5717972/
[6] Wolin, K. Y., GRUBB III, R. L., Pakpahan, R., Ragard, L., Mabie, J., Andriole, G. L., & Sutcliffe, S. (2015). Physical activity and benign prostatic hyperplasia-related outcomes and nocturia. Medicine and science in sports and exercise, 47(3), 581: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4342314/
[7] Kopp, W. (2018). Diet-induced hyperinsulinemia as a key factor in the etiology of both benign prostatic hyperplasia and essential hypertension? Nutrition and Metabolic Insights, 11, 1178638818773072: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6238249/
[8] Vikram, A., Jena, G., & Ramarao, P. (2010). Insulin-resistance and benign prostatic hyperplasia: the connection. European journal of pharmacology, 641(2-3), 75-81: https://pubmed.ncbi.nlm.nih.gov/20553919/
[9] Hammarsten, J., & Högstedt, B. (2001). Hyperinsulinaemia as a risk factor for developing benign prostatic hyperplasia. European urology, 39(2), 151-158: https://pubmed.ncbi.nlm.nih.gov/11223674/
[10] Nandeesha, H., Koner, B. C., Dorairajan, L. N., & Sen, S. K. (2006). Hyperinsulinemia and dyslipidemia in non- diabetic benign prostatic hyperplasia. Clinica chimica acta, 370(1-2), 89-93: https://pubmed.ncbi.nlm.nih.gov/16516184/
[11] Dahle, S. E., Chokkalingam, A. P., Gao, Y. T., Deng, J., Stanczyk, F. Z., & Hsing, A. W. (2002). Body size and serum levels of insulin and leptin in relation to the risk of benign prostatic hyperplasia. The Journal of urology, 168(2), 599-604: https://pubmed.ncbi.nlm.nih.gov/12131317/
[12] Sreenivasulu, K., Nandeesha, H., Dorairajan, L. N., Rajappa, M., & Vinayagam, V. (2017). Elevated insulin and reduced insulin like growth factor binding protein-3/prostate specific antigen ratio with increase in prostate size in Benign Prostatic Hyperplasia. Clinica Chimica Acta, 469, 37-41: https://pubmed.ncbi.nlm.nih.gov/28300542/
[13] Ibero-Baraibar, I., Cuervo, M., Navas-Carretero, S., Abete, I., Zulet, M., & Martinez, J. A. (2014). Different postprandial acute response in healthy subjects to three strawberry jams varying in carbohydrate and antioxidant content: a randomized, crossover trial. European journal of nutrition, 53(1), 201-210: https://pubmed.ncbi.nlm.nih.gov/26376619/
[14] van Buul, V. J., Tappy, L., & Brouns, F. J. (2014). Misconceptions about fructose-containing sugars and their role in the obesity epidemic. Nutrition research reviews, 27(1), 119-130: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4078442/
[15] Claesson, A. L., Holm, G., Ernersson, Å., Lindström, T., & Nystrom, F. H. (2009). Two weeks of overfeeding with candy, but not peanuts, increases insulin levels and body weight. Scandinavian journal of clinical and laboratory investigation, 69(5), 598-605: https://pubmed.ncbi.nlm.nih.gov/19396658/
[16] Stanhope, K. L. (2016). Sugar consumption, metabolic disease and obesity: The state of the controversy. Critical reviews in clinical laboratory sciences, 53(1), 52-67: https://pubmed.ncbi.nlm.nih.gov/26376619/
[17] López-Alarcón, M., Perichart-Perera, O., Flores-Huerta, S., Inda-Icaza, P., Rodríguez-Cruz, M., Armenta-Álvarez, A., … & Mayorga-Ochoa, M. (2014). Excessive refined carbohydrates and scarce micronutrients intakes increase inflammatory mediators and insulin resistance in prepubertal and pubertal obese children independently of obesity. Mediators of inflammation, 2014: https://pubmed.ncbi.nlm.nih.gov/25477716/
[18] Silva, F. M., Kramer, C. K., Crispim, D., & Azevedo, M. J. (2015). A high–glycemic index, low-fiber breakfast affects the postprandial plasma glucose, insulin, and ghrelin responses of patients with type 2 diabetes in a randomized clinical trial. The Journal of nutrition, 145(4), 736-741: https://pubmed.ncbi.nlm.nih.gov/25833777/
[19] Bacchetti, T., Saturni, L., Turco, I., & Ferretti, G. (2014). The postprandial glucose response to some varieties of commercially available gluten-free pasta: a comparison between healthy and celiac subjects. Food & function, 5(11), 3014-3017: https://pubmed.ncbi.nlm.nih.gov/25255330/
[20] Sheard, N. F., Clark, N. G., Brand-Miller, J. C., Franz, M. J., Pi-Sunyer, F. X., Mayer-Davis, E., … & Geil, P. (2004). Dietary carbohydrate (amount and type) in the prevention and management of diabetes: a statement by the American Diabetes Association. Diabetes care, 27(9), 2266-2271: https://diabetesjournals.org/care/article/27/9/2266/22648/Dietary-Carbohydrate-Amount-and-Type-in-the
[21] Messina, M. (2016). Soy and health update: evaluation of the clinical and epidemiologic literature. Nutrients, 8(12), 754: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5188409/
[22] Ajayi, A., & Abraham, K. (2018). Understanding the role of estrogen in the development of benign prostatic hyperplasia. African Journal of Urology, 24(2), 93-97: https://www.sciencedirect.com/science/article/pii/S1110570418300055
[23] Rastrelli, G., Vignozzi, L., Corona, G., & Maggi, M. (2019). Testosterone and benign prostatic hyperplasia. Sexual Medicine Reviews, 7(2), 259-271: https://www.sciencedirect.com/science/article/abs/pii/S2050052118301434
[24] Baas, W., & Köhler, T. S. (2016). Testosterone replacement therapy and voiding dysfunction. Translational Andrology and Urology, 5(6), 890: https://tau.amegroups.com/article/view/11491/13171
[25] Xia, B. W., Zhao, S. C., Chen, Z. P., Chen, C., Liu, T. S., Yang, F., & Yan, Y. (2021). Relationship between serum total testosterone and prostate volume in aging men. Scientific Reports, 11(1), 1-7: https://www.nature.com/articles/s41598-021-93728- 1#:~:text=Current%20studies%20have%20found%20that,response%20in%20the%20prostate19
[26] Yakoob, M. Y., Shi, P., Willett, W. C., Rexrode, K. M., Campos, H., Orav, E. J., … & Mozaffarian, D. (2016). Circulating biomarkers of dairy fat and risk of incident diabetes mellitus among men and women in the United States in two large prospective cohorts. Circulation, 133(17), 1645-1654: https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.115.018410
[27] Imamura, F., Fretts, A., Marklund, M., Ardisson Korat, A. V., Yang, W. S., Lankinen, M., … & Fatty Acids and Outcomes Research Consortium (FORCE). (2018). Fatty acid biomarkers of dairy fat consumption and incidence of type 2 diabetes: a pooled analysis of prospective cohort studies. PLoS medicine, 15(10), e1002670: https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002670
[28] Kratz, M., Baars, T., & Guyenet, S. (2013). The relationship between high-fat dairy consumption and obesity, cardiovascular, and metabolic disease. European journal of nutrition, 52(1), 1-24: https://pubmed.ncbi.nlm.nih.gov/22810464/
[29] Hibbeln, J. R., Nieminen, L. R., Blasbalg, T. L., Riggs, J. A., & Lands, W. E. (2006). Healthy intakes of n− 3 and n–6 fatty acids: estimations considering worldwide diversity. The American journal of clinical nutrition, 83(6), 1483S- 1493S: https://pubmed.ncbi.nlm.nih.gov/16841858/
[30] Rafraf, M., Mohammadi, E., Asghari-Jafarabadi, M., & Farzadi, L. (2012). Omega-3 fatty acids improve glucose metabolism without effects on obesity values and serum visfatin levels in women with polycystic ovary syndrome. Journal of the American College of Nutrition, 31(5), 361-368: https://pubmed.ncbi.nlm.nih.gov/23529993/
[31] Juárez‐López, C., Klünder‐Klünder, M., Madrigal‐Azcárate, A., & Flores‐Huerta, S. (2013). Omega‐3 polyunsaturated fatty acids reduce insulin resistance and triglycerides in obese children and adolescents. Pediatric diabetes, 14(5), 377-383: https://pubmed.ncbi.nlm.nih.gov/23438101/
[32] Samimi, M., Jamilian, M., Asemi, Z., & Esmaillzadeh, A. (2015). Effects of omega-3 fatty acid supplementation on insulin metabolism and lipid profiles in gestational diabetes: Randomized, double-blind, placebo-controlled trial. Clinical Nutrition, 34(3), 388-393: https://pubmed.ncbi.nlm.nih.gov/24973862/
[33] Goldenberg, J. Z., Day, A., Brinkworth, G. D., Sato, J., Yamada, S., Jönsson, T., … & Johnston, B. C. (2021). Efficacy and safety of low and very low carbohydrate diets for type 2 diabetes remission: systematic review and meta- analysis of published and unpublished randomized trial data. bmj, 372: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7804828/
[34] Volek, J. S., Phinney, S. D., Forsythe, C. E., Quann, E. E., Wood, R. J., Puglisi, M. J., … & Feinman, R. D. (2009). Carbohydrate restriction has a more favorable impact on the metabolic syndrome than a low fat diet. Lipids, 44(4), 297-309: https://pubmed.ncbi.nlm.nih.gov/19082851/
[35] Gower, B. A., Chandler‐Laney, P. C., Ovalle, F., Goree, L. L., Azziz, R., Desmond, R. A., … & Bates, G. W. (2013). Favourable metabolic effects of a eucaloric lower‐carbohydrate diet in women with PCOS. Clinical endocrinology, 79(4), 550-557: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4111472/
[36] Barnosky, A. R., Hoddy, K. K., Unterman, T. G., & Varady, K. A. (2014). Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings. Translational Research, 164(4), 302-311: https://pubmed.ncbi.nlm.nih.gov/24993615/
[37] Gabel, K., Kroeger, C. M., Trepanowski, J. F., Hoddy, K. K., Cienfuegos, S., Kalam, F., & Varady, K. A. (2019). Differential effects of alternate-day fasting versus daily calorie restriction on insulin resistance. Obesity, 27(9), 1443-1450: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7138754/
[38] National Center for complementary and integrative Health (NCCIH): https://www.nccih.nih.gov/health/saw- palmetto
[39] Keehn, A., & Lowe, F. C. (2015). Complementary and alternative medications for benign prostatic hyperplasia. Can J Urol, 22(Suppl 1), 18-23: https://www.canjurol.com/html/free- articles/JUV22I5S1F_08_DrLowe.pdf
[40] Khalafi-Kheydani, A., Mahmoodi, H., Sadat, Z., & Azizi-Fini, I. (2022). The effect of nettle root extract on urinary problems in older men with benign prostatic hyperplasia: A randomized clinical trial. Journal of Herbal Medicine, 100568: https://www.sciencedirect.com/science/article/abs/pii/S2210803322000379
[41] Penugonda, K., & Lindshield, B. L. (2013). Fatty acid and phytosterol content of commercial saw palmetto supplements. Nutrients, 5(9), 3617-3633: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3798925/
[42] MacDonald, R., Ishani, A., Rutks, I., & Wilt, T. J. (2000). A systematic review of Cernilton for the treatment of benign prostatic hyperplasia. BJU international, 85(7), 836-841: https://pubmed.ncbi.nlm.nih.gov/10792162/
★ Get My Books - 100% FREE:
😳 Tinnitus And Brain Health?
After 47 years of studies and countless brain scans done on more than 2,400 tinnitus patients, scientists at the MIT Institute found that in a shocking 96% of cases, tinnitus was actually shrinking their brain cells.
As it turns out, tinnitus and brain health are strongly linked.
Even more interesting: The reason why top army officials are not deaf after decades of hearing machine guns, bombs going off and helicopter noises…
Is because they are using something called "the wire method", a simple protocol inspired by a classified surgery on deaf people from the 1950s...
★ How To Get Rid Of Nail Fungus:
★ Does Your Salad Contain This Vegetable?
★ 20 Natural Painkillers In Your Kitchen (Video):
★ Men's Prostate Health:
2. Famous Chef Sheds 60lbs Researching New Paleo Recipes: Get The Cookbook FREE Here
3. #1 muscle that eliminates joint and back pain, anxiety and looking fat
4. 7 odd foods that KILL your abdominal fat (surprising fat-fighters)
5. The TRUTH about bread (Will surprise you!)
6. [PROOF] Reverse Diabetes with a "Pancreas Jumpstart"
7. Here's What Happens When You "Unlock Your Hip Flexors"
8. The #1 WORST food that CAUSES Faster Aging (beware -- Are you eating this?)
The #1 Muscle That Eliminates Joint And Back Pain, Anxiety And Looking Fat
By Mike Westerdal CPT
Can you guess which muscle in your body is the #1 muscle that eliminates joint and back pain, anxiety and looking fat?
This is especially important if you spend a significant amount of time sitting every day (I do, and this really affects me in a big way!)
Working this "hidden survival muscle" that most people are simply not training because no-one ever taught them how will boost your body shape, energy levels, immune system, sexual function, strength and athletic performance when unlocked.
If this "hidden" most powerful primal muscle is healthy, we are healthy.
Is it...
a) Abs
b) Chest
c) Glutes
d) Hip Flexors
Take the quiz above and see if you got the correct answer!
P.S. Make sure you check out this page to get to know the 10 simple moves that will bring vitality back into your life:
If you enjoyed this page: